Professional, Knowledgeable,
Eligibility verification Service
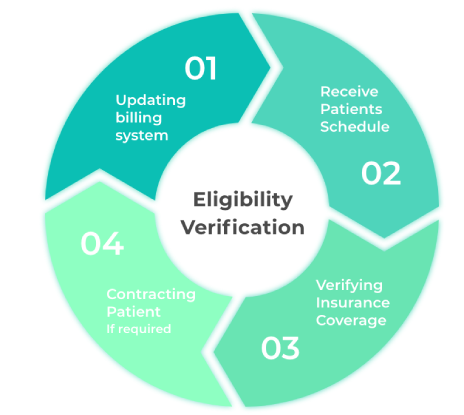
Swagpro Medical Billing Services verification of insurance benefits service standardizes admission processes to improve patient flow. As your authoritative source, we will navigate through the misinformation that is often provided by carriers and guide you through the proper documentation for a thorough utilization review. Insurance eligibility verification is the first and most important step in the medical billing process. The verification of benefits has evolved well beyond deductibles and co-pays. It’s no longer a simple eligibility check. It requires an experienced staff who will work with you directly, and who understands payer benefit systems to eliminate the risk of inaccurate, incomplete, or out-of-date information. As the behavioral healthcare industry grows, insurance carriers are decreasing the number of claims they are paying. For many, this makes verifying benefits challenging. With carriers adding layers of criteria to individual benefit plans, it’s difficult to avoid administrative and financial errors without the help of a verification specialist.
Our verification specialists provide following services:
- Patient policy deductible and out-of-pocket responsibility
- Co-insurance and co-payments
- Benefit limits
- Reimbursement estimates
- Pre-authorization and clinical requirements for admissions
Eliminate errors for faster turnaround times
Verification and eligibility of benefits must be timely and accurate in order to increase your admissions and to maintain a competitive edge. Billing Solutions has years of clinical experience, allowing us to apply our expertise to create a verification of benefits process that differs from other billing companies.
We provide each client with an insurance verification form, specifically tailored to ensure we obtain all necessary information, eliminate the occurrence of errors and aid in a seamless admission process. After providing us with patient and insurance information, you’ll submit the information to our verification team. Our verification specialists confirm the benefits, via online portals and by phone to improve accuracy. Billing Solutions typically returns your completed verification in as little as one hour.
Ongoing clinical reviews
It’s imperative that all benefit information be verified before offering advisement. However, confirming that there are no changes to a client’s benefits during their stay is just as crucial as when they first arrive at your facility.
Therefore, we offer ongoing clinical reviews of your clients’ insurance carriers while they are with you. Conducting clinical reviews guarantees the information you received initially remains accurate and up-to-date, and avoids the high risk of error. We help you plan to re-verify and determine what may have changed with each patient’s benefits. This process solidifies your verification process so you can provide the highest-level of service and extend the length of client stays, all while we keep the insurance provider accountable.
Swagpro Medical Billing Services is a customer-centric company. We can provide your organization greatest financial return through our services. We’re transparent, dependable and responsive to your needs. Our goal is to make your organization run smoother and efficient. Like many other companies, we’re not focused on selling you other products. Our exclusive focus is on the revenue cycle management and collect the maximum revenue for your organization. We have a strong team of billers, coders and A/R specialists. Most of our clients who switched from other billing companies to us were only getting mediocre services. Swagpro Medical Billing Services makes sure that all our clients get top quality medical billing and AR follow up services while they focus on what mat
EMR/EHR services | Medical billing services in Nebraska | Revenue cycle management service Provider | Medical Coding services